This vaccine has not been approved or licensed, and is still under investigation.1
Janssen (Johnson & Johnson) COVID-19 Vaccine:
Short-Term Efficacy & Safety Data
 1. WHAT IS THE JANSSEN (JOHNSON & JOHNSON) COVID-19 VACCINE?
1. WHAT IS THE JANSSEN (JOHNSON & JOHNSON) COVID-19 VACCINE?
The Janssen (Johnson & Johnson) COVID-19 vaccine (Ad26.COV2.S) is made from inactivated adenovirus viral particles that are modified to include genetic material that codes for part of the SARS-CoV-2 virus, the virus that can cause COVID-19. More specifically, DNA that codes for a mutated spike (S) protein of the SARS-CoV-2 virus is embedded into inactivated adenovirus viral particles and grown in a fetal cell line. The drug is administered in one intramuscular dose of 50 billion viral particles.1
 2. HOW WAS THE VACCINE STUDIED PRIOR TO OBTAINING EUA?
2. HOW WAS THE VACCINE STUDIED PRIOR TO OBTAINING EUA?
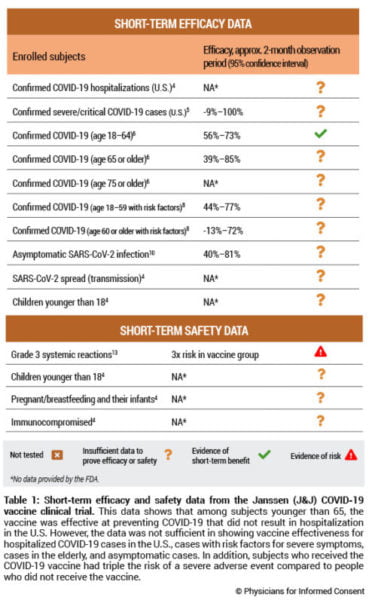
The Janssen COVID-19 vaccine has obtained emergency use authorization (EUA) from the U.S. Food and Drug Administration (FDA) and is currently investigational.2 The vaccine was studied through nonclinical data from mice, rabbits, hamsters and nonhuman primates, and clinical data from humans.3 The EUA was based on a human clinical trial comparing approximately 22,000 subjects who received the vaccine with 22,000 subjects who did not receive the vaccine (Table 1).4 The trial included a median observation period of eight weeks; 54.6% of subjects were followed up for at least eight weeks after vaccination.4 The FDA states that due to the length of the clinical trial’s observation period, “it is not possible to assess sustained efficacy over a period longer than 2 months.”4
 3. DOES THE VACCINE PREVENT HOSPITALIZATIONS AND DEATHS?
3. DOES THE VACCINE PREVENT HOSPITALIZATIONS AND DEATHS?
The FDA states, “The totality of these data indicates vaccine efficacy in the prevention of severe COVID-19 requiring hospitalization.”4 However, more than 60% (26 of 43) of the severe/critical cases were observed in South Africa, whereas less than 19% (8 of 43) were observed in the U.S.5 The fact that severe/critical COVID-19 is more than four times more likely to occur in South Africa (26 of 113) than in the U.S.
(8 of 152) suggests that conditions in the U.S. reduce the severity of COVID-19. Since only eight severe/critical cases of COVID-19 were observed in the U.S. at least 28 days after vaccination, the clinical trial did not have enough statistical power to measure the vaccine’s ability to prevent hospitalizations from COVID-19 in the U.S.5 See Table 1. There were also no COVID-19 deaths observed in the U.S., and the FDA states, “A larger number of individuals at high risk of COVID-19 and higher attack rates would be needed to confirm efficacy of the vaccine against mortality.”4
 4. HOW EFFECTIVE IS THE VACCINE IN ADULTS AND THE ELDERLY?
4. HOW EFFECTIVE IS THE VACCINE IN ADULTS AND THE ELDERLY?
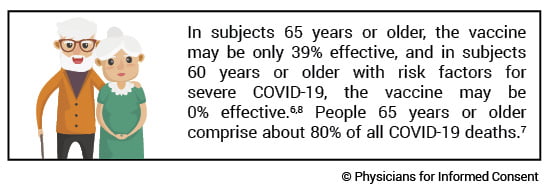
Vaccine effectiveness was calculated by observing the vaccination status of 437 COVID-19 cases, where a COVID-19 case was defined as a positive SARS-CoV-2 test and the presence of either two typical COVID-19 symptoms or one or more severe COVID-19 symptoms. In subjects 18 to 64 years old, the vaccine was 56%–73% effective against cases occurring at least 28 days after vaccination.6 However, since there were only 46 COVID-19 cases observed in subjects 65 to 74 years old and only four cases in subjects 75 years or older, the clinical trial did not have enough statistical power to accurately measure the vaccine’s effectiveness in those age groups. The vaccine may be only 39% effective in subjects 65 years or older and 0% effective in subjects 75 years or older.6 See Table 1. Subjects 65 years or older comprise about 80% of all COVID-19 deaths, and subjects 75 years or older comprise about 60% of all COVID-19 deaths.7
The clinical trial also included an analysis of vaccine effectiveness for subjects with risk factors making them more vulnerable to severe COVID-19 symptoms, such as obesity, diabetes, and hypertension. In subjects 18 to 59 years old with these risk factors, the vaccine was 44%–77% effective against cases occurring at least 28 days after vaccination.8 However, since there were only 41 COVID-19 cases observed in subjects 60 years or older, the clinical trial did not have enough statistical power to accurately measure the vaccine’s effectiveness in that age group. The vaccine may be 0% effective in subjects 60 years or older with risk factors.8 See Table 1.
Of note, the clinical trial also included over 2,000 unvaccinated subjects that had contracted SARS-CoV-2 before the study. The trial recorded the incidence of COVID-19 in that group at least 28 days after the vaccination of the other subjects in the study. The COVID-19 incidence of the group with prior SARS-CoV-2 infection was 0.1% (2/2,021), whereas the COVID-19 incidence of vaccinated subjects was 0.59% (113/19,306).9 These data suggest that there are six times more cases of COVID-19 in vaccinated subjects than in subjects previously infected with SARS-CoV-2.
 5. IS THE VACCINE EFFECTIVE IN CHILDREN?
5. IS THE VACCINE EFFECTIVE IN CHILDREN?
Efficacy data was not available and safety data was insufficient in children younger than 18 years.4 See Table 1.
 6. IS THE VACCINE EFFECTIVE IN PREVENTING INFECTION WITH SARS-COV-2 OR THE SPREAD OF COVID-19?
6. IS THE VACCINE EFFECTIVE IN PREVENTING INFECTION WITH SARS-COV-2 OR THE SPREAD OF COVID-19?
The FDA states, “The evaluation of vaccine efficacy against asymptomatic disease and its interpretation are limited at this time, since the measurements were performed in a small subset of participants.” The trial only analyzed about 2,600 subjects for the potential of asymptomatic infection and found 18 cases in the vaccinated group and 50 cases in the unvaccinated group, resulting in a vaccine effectiveness potentially as low as 40%.10 See Table 1. Consequently, the FDA states that “it is possible that asymptomatic infections may not be prevented as effectively as symptomatic infections” and “data are limited to assess the effect of the vaccine against transmission of SARS-CoV-2 from individuals who are infected despite vaccination.” Furthermore, “additional evaluations including data from clinical trials and from vaccine use post-authorization will be needed to assess the effect of the vaccine in preventing virus shedding and transmission, in particular in individuals with asymptomatic infection.”4
Of note, the 50 asymptomatic cases described above comprised 3.8% of the 1,304 unvaccinated subjects included in that analysis.10 The trial also recorded 432 unvaccinated symptomatic COVID-19 cases confirmed by a central laboratory.11 Since such cases comprised 68% of all COVID-19 cases that tested positive for SARS-CoV-2,4 the trial recorded an estimated 635 (432/68%) symptomatic COVID-19 cases among 19,544 unvaccinated subjects (3.25%).12 These data suggest that 54% (3.8%/[3.25%+3.8%]) of all COVID-19 cases in the clinical trial were asymptomatic.
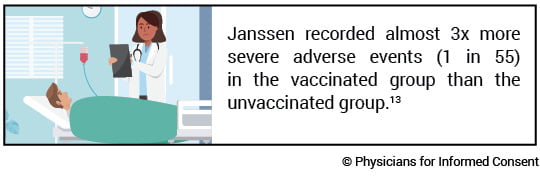
 7. WHAT IS THE RISK OF A SEVERE SIDE EFFECT FROM THE VACCINE?
7. WHAT IS THE RISK OF A SEVERE SIDE EFFECT FROM THE VACCINE?
The Janssen COVID-19 vaccine clinical trial found the overall incidence of grade 3 systemic adverse events within seven days of vaccination to be 1.8% or 1 in 55 in the vaccinated group and 0.6% in the unvaccinated group, resulting in a vaccine risk of 1.2% or 1 in 84 vaccinated subjects.13 Consequently, subjects who received the vaccine had about triple the risk of a grade 3 systemic adverse event within seven days of vaccination compared to subjects who did not receive the vaccine. See Table 1. Systemic adverse events included fatigue, headache, myalgia, nausea, and fever.4 A grade 3 adverse event is a severe event that prevents the ability to perform normal daily activities, including work, and requires medical attention.14
Additionally, as there were only 5,031 subjects 18 to 39 years of age who received the vaccine,3 and since as of March 23, 2021, about 1 in 13,000 people 18 to 39 years of age contracted a fatal case of COVID-19 in the U.S.,7 the clinical trial does not have sufficient data to determine safety in subjects who are 18 to 39 years of age. Per the FDA, “There are currently insufficient data to make conclusions about the safety of the vaccine in subpopulations such as children less than 18 years of age, pregnant and lactating individuals and their infants, and immunocompromised individuals.”4 And, because all subjects were observed for only two months, the long-term safety of the vaccine for any age group is not known.
 8. IS THE COVID-19 VACCINE EFFECTIVE AND SAFER THAN COVID-19?
8. IS THE COVID-19 VACCINE EFFECTIVE AND SAFER THAN COVID-19?
The extent to which the Janssen COVID-19 vaccine is effective and safer than COVID-19 is not known. The clinical trial indicates that in subjects 65 years or older, the vaccine may be only 39% effective, and in subjects 75 years or older, the age group that comprises about 60% of all COVID-19 deaths, the vaccine may be 0% effective; also, in subjects 60 years or older with risk factors for severe COVID-19 the vaccine may not be effective. The clinical trial did not have enough statistical power to measure the vaccine’s ability to prevent hospitalizations and deaths in the U.S., and the trial had limited data to assess whether the vaccine prevents asymptomatic infection or spread (transmission) of the virus.
Grade 3 systemic adverse events in the vaccine group occurred in 1 in 55 subjects in the Janssen clinical trial. Furthermore, for people 18 to 39 years of age, the clinical trial did not include enough subjects to be able to show that the vaccine is safer than the disease, and because the clinical trial observation period lasted only two months, the incidence of long-term side effects from the vaccine for any age group is not known.
REFERENCES
-
U.S. Food and Drug Administration, Vaccines and Related Biological Products Advisory Committee. FDA briefing document: Emergency use authorization (EUA) for an unapproved product—review memorandum. Janssen Ad26.COV2.S (COVID-19) vaccine. 2021 Feb 4. https://www.fda.gov/media/146338/download.
-
Hinton, Denise M. (U.S . Food and Drug Administration). Letter to: Ruta Walawalkar (Janssen Biotech, Inc.). 2021 Feb 27. https://www.fda.gov/media/146303/download.
-
Janssen Biotech, Inc. Janssen Biotech, Inc. COVID-19 vaccine Ad26.COV2.S: VAC31518 (JNJ-78436735). Vaccines and Related Biological Products Advisory Committee sponsor briefing document. Meeting date: 26 February 2021: 13, 31, 109. https://www.fda.gov/media/146219/download.
-
U.S. Food and Drug Administration, Vaccines and Related Biological Products Advisory Committee. FDA briefing document: Janssen Ad26.COV2.S vaccine for the prevention of COVID-19. Vaccines and Related Biological Products Advisory Committee Meeting: February 26, 2021: 12-15, 17, 19, 25, 27, 29, 31, 33, 35, 37-39, 41, 56-57. https://www.fda.gov/media/146217/download.
-
U.S. Food and Drug Administration, Vaccines and Related Biological Products Advisory Committee. FDA briefing document: Janssen Ad26.COV2.S vaccine for the prevention of COVID-19. Vaccines and Related Biological Products Advisory Committee Meeting: February 26, 2021. Table 22: vaccine efficacy of first occurrence of moderate to severe/critical and severe/critical COVID-19 including non-centrally confirmed cases with onset at least 14 or at least 28 days after vaccination, by country of participation, per-protocol set, study 3001; 37. https://www.fda.gov/media/146217/download.
-
U.S. Food and Drug Administration, Vaccines and Related Biological Products Advisory Committee. FDA briefing document: Janssen Ad26.COV2.S vaccine for the prevention of COVID-19. Vaccines and Related Biological Products Advisory Committee Meeting: February 26, 2021. Table 12: vaccine efficacy of first occurrence of moderate to severe/critical COVID-19, including non-centrally confirmed cases, with onset at least 14 or at least 28 days after vaccination, by demographic characteristics, per-protocol set, study 3001; 27, 28. https://www.fda.gov/media/146217/download.
-
Centers for Disease Control and Prevention. Washington, D.C.: U.S. Department of Health and Human Services. Weekly updates by select demographic and geographic characteristics: provisional death counts for coronavirus disease (COVID-19); [cited 2021 Mar 23]. https://www.cdc.gov/nchs/nvss/vsrr/covid_weekly/index.htm#AgeAndSex.
-
U.S. Food and Drug Administration, Vaccines and Related Biological Products Advisory Committee. FDA briefing document: Janssen Ad26.COV2.S vaccine for the prevention of COVID-19. Vaccines and Related Biological Products Advisory Committee Meeting: February 26, 2021. Table 13: vaccine efficacy of first occurrence of moderate to severe/critical COVID-19, including non-centrally confirmed cases, with onset at least 14 or at least 28 days after vaccination, by risk factors for severe COVID-19, per-protocol set, study 3001; 29, 30. https://www.fda.gov/media/146217/download.
-
U.S. Food and Drug Administration, Vaccines and Related Biological Products Advisory Committee. FDA briefing document: Janssen Ad26.COV2.S vaccine for the prevention of COVID-19. Vaccines and Related Biological Products Advisory Committee Meeting: February 26, 2021. Table 14: vaccine efficacy of first occurrence of moderate to severe/critical COVID-19, including non-centrally confirmed cases, with onset at least 14 or at least 28 days after vaccination, by baseline SARS-CoV-2 status, per protocol set; 30. https://www.fda.gov/media/146217/download.
-
U.S. Food and Drug Administration, Vaccines and Related Biological Products Advisory Committee. FDA briefing document: Janssen Ad26.COV2.S vaccine for the prevention of COVID-19. Vaccines and Related Biological Products Advisory Committee Meeting: February 26, 2021. Table 20: vaccine efficacy against asymptomatic SARS-CoV-2 infections, full analysis set; 35, 36. https://www.fda.gov/media/146217/download.
-
U.S. Food and Drug Administration, Vaccines and Related Biological Products Advisory Committee. FDA briefing document: Janssen Ad26.COV2.S vaccine for the prevention of COVID-19. Vaccines and Related Biological Products Advisory Committee Meeting: February 26, 2021. Figure 1: cumulative incidence curve of centrally confirmed moderate to severe/critical COVID-19 cases with onset at least 1 day after vaccination, full analysis set; 31. https://www.fda.gov/media/146217/download.
-
U.S. Food and Drug Administration, Vaccines and Related Biological Products Advisory Committee. FDA briefing document: Janssen Ad26.COV2.S vaccine for the prevention of COVID-19. Vaccines and Related Biological Products Advisory Committee Meeting: February 26, 2021. Table 10: vaccine efficacy against centrally confirmed moderate to severe/critical COVID-19 with onset at least 14 and at least 28 days after vaccination, per-protocol set, study 3001; 25. https://www.fda.gov/media/146217/download.
-
U.S. Food and Drug Administration, Vaccines and Related Biological Products Advisory Committee. FDA briefing document: Janssen Ad26.COV2.S vaccine for the prevention of COVID-19. Vaccines and Related Biological Products Advisory Committee Meeting: February 26, 2021. Table 23: participants reporting at least one adverse event, among all participants and by age group; 39, 40. https://www.fda.gov/media/146217/download.
-
U.S. Department of Health and Human Services. Washington, D.C.: U.S. Department of Health and Human Services. Common terminology criteria for adverse events (CTCAE); 2017 Nov 27. https://ctep.cancer.gov/protocoldevelopment/electronic_applications/docs/CTCAE_v5_Quick_Reference_8.5×11.pdf.
These statements are intended for informational purposes only and should not be construed as personal medical advice.
© 2021 Physicians for Informed Consent, an independent 501(c)(3) nonprofit educational organization. All rights reserved. May 2021.